Puzzled by Pain
Think about a large, complicated, one-thousand-piece puzzle. If you look at a single piece, it does not usually create a picture.

But once surrounded by several other pieces, it begins to take shape and look like the picture on the box.

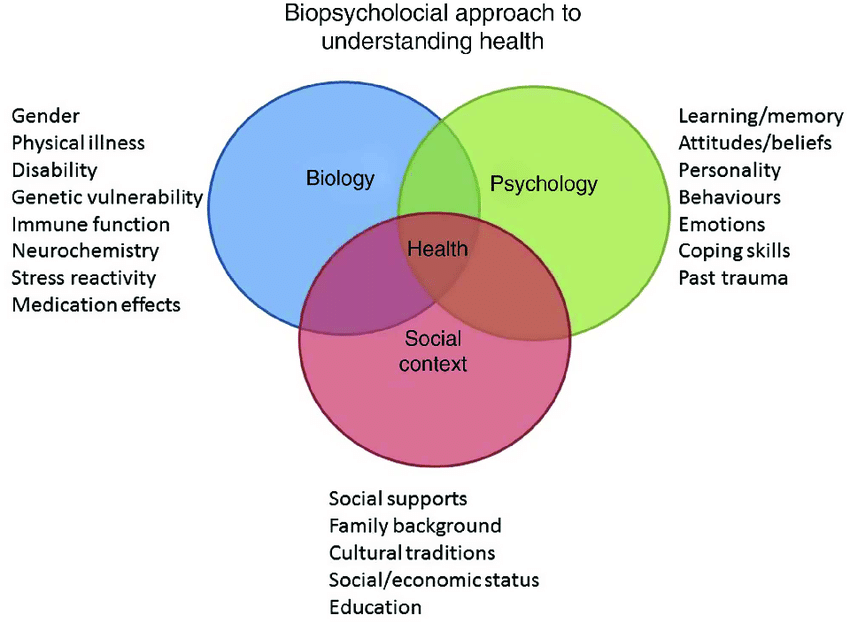
These surrounding puzzle pieces have an influence on how you perceive the single piece. Similarly, we are influenced by what is around us as well as what is within us, and this is called the Bio-psycho-social Model.
(Levy-Storms, 2018)
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, living within this puzzle known as the Biopsychosocial Model (Shmidt, 2019). See previous posts to refresh on the concept how pain relates (or does not relate) to tissue damage. Your puzzle pieces include:
- Biology tends to be the first thing we think of in terms of our health and what causes our pain. For instance, we may think first about a broken bone, a cut or bruise, nerve damage, tendinopathy, etc. However, pain is more than just damaged tissues; remember that bruise that seemed to pop up out of nowhere?
- A less obvious example of how biology relates to pain is immune cells, which can enhance your danger detection system. This is one reason we feel more aches and pains when we are sick (Moseley & Butler, 2017).
- Psychology also plays a significant role not only in how we feel, but what we feel. Psychology includes your personality, motivation, health beliefs, coping styles, and emotions. Even past traumas can affect how you perceive pain.
- Let us imagine a traumatic car accident where you had soreness in your neck afterwards. The stress hormones related to the psychological trauma will enhance your danger detection system. If you are on a nerve-racking car ride in the future, the stress hormones alone can activate your danger detectors and cause pain in your neck, without physical damage to cause the pain (Moseley & Butler, 2017).
- An example of the influence of motivation and emotions may be a headache. This will hurt less when you are having fun with people you enjoy than when attending a meeting that could have been an email.
- Social aspects of our life often get forgotten when thinking about health and pain. This involves the world around us, family, friends, economic status, cultural traditions, etc. Maybe the social realm became more important recently in regards to the Coronavirus; it is important to restrict our social interactions to slow the spread of the virus, but we may notice our mental health degrading without being able to interact with friends and family. The Social piece of the puzzle can be the positive support system of your spouse, or it can be the negative influence of your friends, or it could be that your cultural beliefs differ from that of your physicians.
- For example, cultural beliefs differ in the acceptance of health-promotion measures (vaccines, birth control), the amount of control an individual feels they have in preventing and controlling health issues, and family dynamics (maternal vs paternal control, gender roles). Even eye contact can be perceived as rude or polite depending on the culture.
When thinking about treatment for pain, we want to try to put your puzzle pieces into one beautiful picture. For the Bio piece, we need to learn to listen to the danger messages our body is sending, and how to interpret overprotective messages. For the psychological and social pieces, it is important to work as a team; having healthcare providers you trust to work with on goals and interventions, and especially having belief in yourself to play an active role in recovery (Zimney, 2019).
Stay tuned for upcoming posts to talk about how to identify helpful and hurtful puzzle pieces and how to use those on the Protectometer.
- Levy-Storms, L., Chen, L., Loukaitou-Sideris, L. (2018). Older Adults’ Needs and Preferences for Open Space and Physical Activity in and Near Parks: A Systematic Review. Journal of Aging and Physical Activity, 26 (4), 682-696.
- Schmidt, S. (2019). Moving Without Moving [Powerpoint Slides]. Retrieved from Align Conference.
- Moseley, G. L. & Butler, D. S. (2017) Explain Pain Supercharged. Noigroup Publications.
- Zimney, K. (2019) Moving Towards the Patient [Powerpoint Slides]. Retrieved from Align Conference.
Post Written by PRO’s Own Sarah Geraghty

